Evidence of mind-body connections suggests vast malleability vis-à-vis modifiable lifestyle factors. Among people affected by Parkinson’s disease (PD), more inclusive clinical interventions need to be adopted, such that non-motor complications are flipped on its head. An area even less studied is the effects of grief. Due to the compounding nature of a pandemic, clinical interventions for treatments of grief as a way of moderating dementia symptoms in PD are needed now more than ever. How are the environment, COVID-19, Parkinson’s and grief all intricately connected?
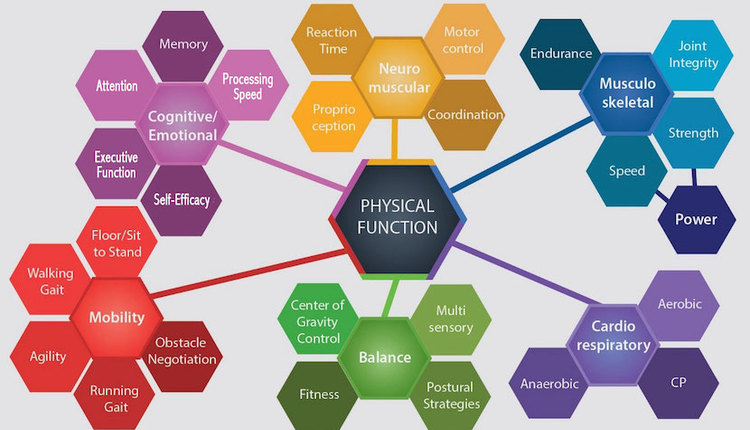
The environment shapes our brain. Grief reshapes our brain. The pandemic has reshaped our environment. According to principal study author Kühn, “brain plasticity supports the assumption that the environment can shape brain structure and function.” Most notably is the effect of the environment on the amygdala. With a healthy functioning amygdala, part of the limbic system and the specific region responsible for emotion regulation, grievers are able to navigate, find and assign meaning in loss episodes. For people with PD, there is an estimated 20% atrophy of their amygdala. How might one’s experience with PD shift positively if fitness and health practitioners allow space for breaching current and residual grief episodes?
Perhaps a starting point could be an inclusion of the Brief Grief Questionnaire (BGQ) in the intake assessment interview. Rather than a standalone instrument, to be completed by the participant prior to meeting, the 5-item screening tool should be delivered in an interview format. Often, grief is underreported, socially and culturally unrecognized and thus untreated. Grief is the antithesis of mind-body homeostasis. Although the BGQ has been developed for measuring and screening for complicated grief, the instrument holds strong reliability and discriminant validity. Complicated grief occurs when the mourning process is interrupted and frozen in the mind-body matrix. Future crisis, as COVID-19 is for some, can possibly unfreeze previous grief episodes and catapult one into the middle of a large body of frigid waters, with no life-saving measures in sight. The BGQ can serve as a life preserver. Participants are prompted to assign a value of “not at all, “somewhat”, or “a lot” to each question. One such question asks:
How much are you having images or thoughts of _____ when he/she/they died or other thoughts about the death that bother you?
Self-reported levels of anxiety are much higher among people diagnosed with PD as compared with their non-PD counterparts, when matched for age, gender, race and socio-economic status. Could it be that anxiety associated with loss and separation in the human need to fulfill attachments, then results in systemic overload and is diagnosed as dementia in PD? The concept of “possible selves” can be used as a template for informing the grieving of the possible selves that one imagined and may never live once diagnosed.
Intake assessments that account for previous life losses, as well as the potential exacerbating loss effects of a PD diagnosis aim to take into account the whole person. Practitioners who fail to contextualize a person’s diagnosis within one’s lived history of losses is systematically failing a PD survivor. It is imperative to adopt a grief lens when working with people experiencing dementia symptoms of PD. Further, we can see where Horchschild’s concept of “feeling rules” dictates the lack of grief that surrounds a diagnosis.
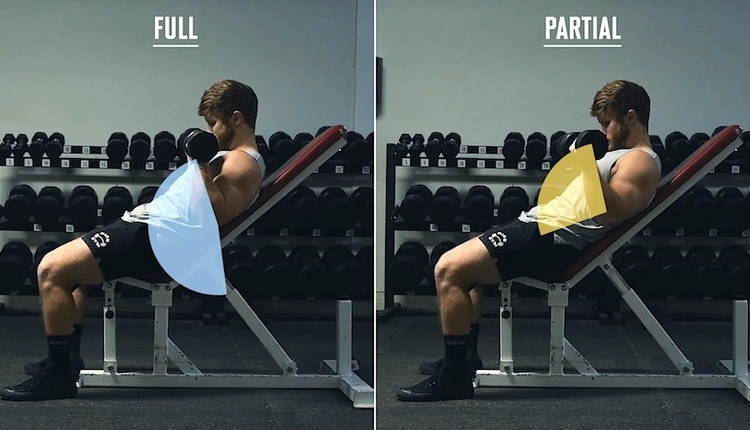
Additionally, exercise programs should consider opportunities for stimulating somatosensory recruitment, which has been suggested to mediate mild cognitive emotional deficits with respect to regulation of the amygdala. Nociception, proprioception, touch and temperature can be assessed in a clear and simple method of inquiry: “How comfortable are you?” Asking this throughout a strength training regimen allows participants to develop new neural pathways that may circumnavigate previously laid and now deteriorating pathways. Could it be that the symptom of dementia in PD is less about the disease and more an outcome of current treatments?
Answering this question is actually less important than considering incorporating the BGQ into your training practices. It’s absurd to think any practicing health and fitness professional is not committed to social justice. In a culture that already denies death, we can play a pivotal role in shifting the dementia divide. Kenneth Doka, Professor Emeritus at the Graduate School of The College of New Rochelle and Senior Consultant to the Hospice Foundation of America offers guidance on adopting a holistic systems approach to life-threatening illness diagnosis. He outlines tasks that can be considered by fitness professionals when supporting participants diagnosed with PD – after first learning their stage: acute, chronic, terminal. Although each task may vary in actualized form depending upon each participant and a professional’s background, three general areas to consider are: ventilating feelings and fears; preserving, redefining self-concept; and examining and maximizing health and lifestyle. Physical activities can be utilized as a vehicle for addressing these areas. One caveat, is that professionals should always operate within their areas of expertise and when appropriate, refer to other professionals.
As you contemplate the responsibility you have in assessing the whole person, consider incorporating novel approaches that value, expose and decomplicate one’s grief – past, present and future. Validating participants grief episodes today, may lead to a more just society tomorrow.