Beyond doing planks, the value of isometric exercises is often overlooked. In fact, isometrics have gained an unfavorable reputation in many training ecosystems with phrases like:
- “Why would you want to cut off blood supply to a working muscle?”
- “There are much better exercises to burn calories.”
- “Isometrics aren’t functional, so they are a waste of time.”
Instead of evaluating isometric exercise value based on common gym phrases, let’s consider what isometrics can do for your clients. Once benefits are clear, isometric exercise selection toward client goals becomes transparent.
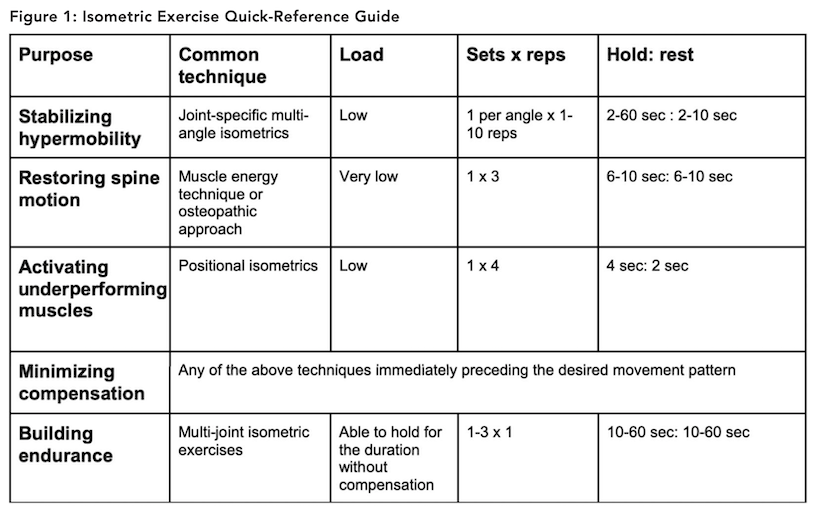
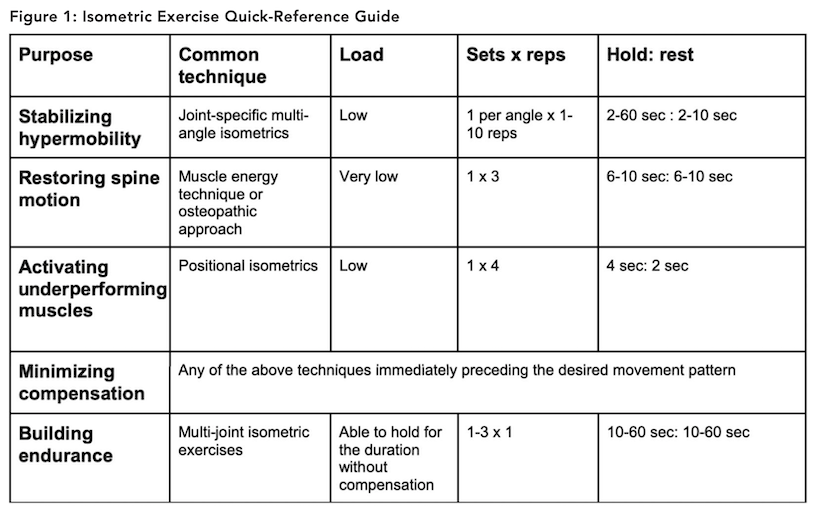
Client benefits from isometric exercise selection can include:
- Stabilizing hypermobilities
- Restoring spine motion
- Activating underperforming muscles
- Minimizing compensation in multi-joint exercises
- Building endurance
Now, let’s discover what clues clients present to help hone in on specific techniques.
GOAL: STABILIZING HYPERMOBILITIES
Client presentation: Clients that benefit from stabilizing hypermobility typically complain of increasing incidents of their “back going out,” or concern that their chiropractic adjustments never seem to hold. Some may have underlying genetic hypermobility. One of the most common underlying diagnoses is Ehler-Danlos.
Key variables to stabilize hypermobilities include:
- Joint specificity: Joint-specific stabilization requires the force to be placed close to the joint of interest. There should not be another joint between the joint of interest and the force application point.
- Very low load: Less is more. Typically, stabilizing isometrics require forces that are a tiny fraction of body weight. The further the resistance is away from the target joint, the lower the force required.
- Multi-angle: Isometric exercises only have a 10-degree carryover. This means that the motion will be strong at the angle at which it is trained, and 10 degrees on either side of the trained position. This is why isometrics typically need to be repeated at several angles throughout the joint’s range of motion.
- Increasing duration: The progression variable is duration. Start with 2-10 second holds, gradually progressing to 30-60 second holds over several weeks.
GOAL: RESTORING SPINE MOTION
Client presentation: Clients present with complaints like “my spine is stuck.” They can show you a spine motion and demonstrate their limitation in one or more directions. If you look closely at each segment of the client’s spine moving, you can often find a segment that doesn’t quite line up with the spinal curve at the sticking point. This is often termed a hypomobile segment or subluxation.
Isometric exercise prescription to restore spine motion
Exercises in this category are often very specific and most typically utilized by allied health providers. These isometrics typically go by names like “osteopathic approach” or muscle energy techniques.
Key variables to restore spine motion include:
Very joint-specific: Allied health providers will work through a process of “locking out” a joint in all three planes of motion, followed by an isometric. After this, the allied health provider takes up any joint slack in each plane, then repeats the process.
Very low load: Forces applied are barely enough to palpate local muscle action around the affected area.
Sets and reps: 1 set of 3 repetitions with a 6-10 second isometric followed by passive movement into the new range is typical for muscle energy techniques. This series is typically followed by carefully controlled active assisted motion, active motion and, finally, lightly resisted motion to encourage normal joint mechanics.
GOAL: ACTIVATE UNDERPERFORMING MUSCLES
Client presentation: Underperforming muscles bring out a variety of client presentations. The power athlete might complain of decreased height when jumping or slowness when performing high-speed lifts. The endurance athlete might complain of a sluggish feeling in working muscles, decreasing speed over time, unusual muscle cramping or the sense that they just can’t feel a muscle performing or activating. On the rehab side, clients present with overuse injuries and biomechanical dysfunction like bursitis, tendinitis, tendinopathy and patellofemoral syndrome.
Key variables to activate underperforming muscles include:
Muscle-specific: Each muscle has a specific 3-dimension-specific position at which its EMG firing pattern supersedes surrounding muscles. In this position, practitioners guide clients through positional isometrics to help the nervous system better recruit the called-upon muscle.
Progressive low load: The load is often progressed within the set over a series of repetitions as follows: 25%, 50%, 75% and 100% maximal voluntary contraction (MVC). 100% maximal voluntary contraction is the point at which the fitness or allied health provider can feel or see the client properly contracting the muscle to stabilize the joint of interest without any compensation into nearby muscles or joints. Many times, this force is less than one pound when it is applied close to the muscle of interest. If the force is applied further away, the force is adjusted downward.
Sets and reps: Sets and reps vary based on the exact positional isometric technique used. 1 set of 4 in a cycle of 4-second isometric hold: 2-second relax represents one common method used by fitness professionals.
Progression: Since isometrics only have a 10-degree carryover, professionals often include multiple increasing joint angles within the isometric section of their program.
GOAL: MINIMIZE COMPENSATION
Client presentation: Compensation is often first detected by the fitness or rehab professional. Continued slight movement deviations despite changes in exercise specifications or cueing appear persistent, even after the client has become aware of more ideal movement patterns. The client simply can’t will his/her body to perform what you ask.
Key variables to minimize compensation include:
Selecting the right activation technique: While all of the techniques work, selecting the ones within the professional’s training level, and the one that creates immediate and lasting change for the client are top choices.
Timing: With the key goal of neuromuscular activation directed at specific joints and muscles, the selected activation technique should immediately precede the desired workout movements.
Cueing: Isometric techniques enhance neuromuscular activation without providing the joints or muscles any instruction on how to work. The subsequent exercise selection, environmental setup, and cue selection should support more ideal movement with less compensation than before the isometrics were performed.
GOAL: BUILD ENDURANCE
Client presentation: Clients often present with postural syndromes like upper-crossed, lower-crossed or pronation distortion syndrome. These are not medical diagnoses, but rather sub-optimal postural patterns associated with the development of pain over time. Many times, clients can be cued out of these postures, but they cannot maintain them for any meaningful duration.
Key variables to build endurance include:
Position: Endurance builders are often multi-joint exercises. Select a position variation that the client can hold with proper muscle recruitment.
Duration: Duration is the most common progression, beginning with 1-3 sets of 10-second holds and progressing toward 1+ minute. Once a client can hold a position for 1 minute without compensating, a gradual external load can offer further progression.
Frequency: Since isometrics do not move joint surfaces, joint sheer and soft tissue breakdown associated with concentric and eccentric exercises are not present. This makes isometric exercise a viable daily option to improve postural and core support muscle endurance.
Putting it all together
While isometric exercise is likely not the best choice for goals like burning a high number of calories in a workout, we can see that different kinds of isometrics can increase movement efficiency. Save Figure 1 as an isometric exercise quick-reference guide to incorporate the ones that match your client’s goals.
Dr. Meredith Butulis, DPT, OCS, CEP, CSCS, CPT, PES, CES, BCS, Pilates-certified, Yoga-certified, has been working in the fitness and rehabilitation fields since 1998. She is the creator of the Fitness Comeback Coaching Certification, author of the Mobility | Stability Equation series, Host of the “Fitness Comeback Coaching Podcast,” and Assistant Professor the State College of Florida. She shares her background to help us reflect on our professional fitness practices from new perspectives that can help us all grow together in the industry. Instagram: @Dr.MeredithButulis.